Magnesium in HTMA: Energy, Stress Resilience & Mineral Balance
Magnesium is one of the most misunderstood minerals in the body.
It’s often described as a “calming supplement” — something you take for sleep, muscle cramps, or anxiety. But in Hair Tissue Mineral Analysis (HTMA), magnesium reveals something far more important: how efficiently your body produces energy, tolerates stress, and recovers over time.
When magnesium is depleted, misused, or locked into an unavailable form, the body struggles to regulate the nervous system, stabilize energy production, and adapt to pressure — even when diet and supplements look “good on paper.”
HTMA helps uncover how magnesium is actually functioning at the tissue level, not just whether you’re getting enough.
Article Contents
- Why Magnesium Matters
- Magnesium & Cellular Energy
- Magnesium–Calcium Balance
- What Magnesium Levels Mean in HTMA
- High vs Low vs Biounavailable Magnesium (Table)
- Magnesium, Oxidation Rate & Stress
- Stress, Inner Pressure & Magnesium Depletion
- What Magnesium Changes Mean on a Retest
- Factors That Deplete or Block Magnesium
- Magnesium Supplementation in Context
- FAQs
- Final Takeaway
Why Magnesium Matters
Magnesium is a primary intracellular mineral, meaning most of its work happens inside your cells.
About 60% of magnesium is stored in bone, while the rest supports thousands of enzymatic reactions related to metabolism, detoxification, hormone signaling, and nervous system regulation.
Magnesium supports:
- Nervous system stability and stress buffering
- Muscle relaxation and prevention of tissue calcification
- Glucose and fat metabolism
- Liver detoxification and protection from heavy metals
- Bone health through calcium regulation
- Kidney health and fluid balance
Because magnesium is used constantly — and lost easily — deficiency or dysfunction is extremely common in modern life.
Magnesium & Cellular Energy
Magnesium is essential for ATP production, the body’s main energy currency.
Inside the mitochondria, magnesium activates ATP and allows it to be used efficiently. Without enough usable magnesium, energy production slows — even if calories, oxygen, and nutrients are present.
Magnesium also has an oxygen-sparing effect, meaning it helps cells generate energy with less metabolic strain. This makes it especially important during periods of chronic stress, illness, or recovery.
When magnesium is impaired:
- Energy feels limited or inconsistent
- Fatigue becomes persistent rather than situational
- Stress recovery slows
- The nervous system becomes more reactive
Magnesium–Calcium Balance
Magnesium and calcium function as regulatory partners.
Calcium provides structure and slowing; magnesium provides flexibility and release. When calcium rises without sufficient magnesium, calcium tends to deposit in soft tissues rather than being used constructively.
An elevated calcium-to-magnesium (Ca/Mg) ratio often signals a relative magnesium deficiency, even when hair magnesium appears normal or high.
This imbalance may contribute to:
- Muscle tightness and cramps
- Joint stiffness or calcification
- Kidney stones
- Heightened stress reactivity
- Reduced stress tolerance
HTMA excels at detecting relative imbalances like this — patterns that blood tests often miss.
What Magnesium Levels Mean in HTMA
HTMA does not label magnesium as simply “low” or “high.”
It shows how magnesium is being used in context.
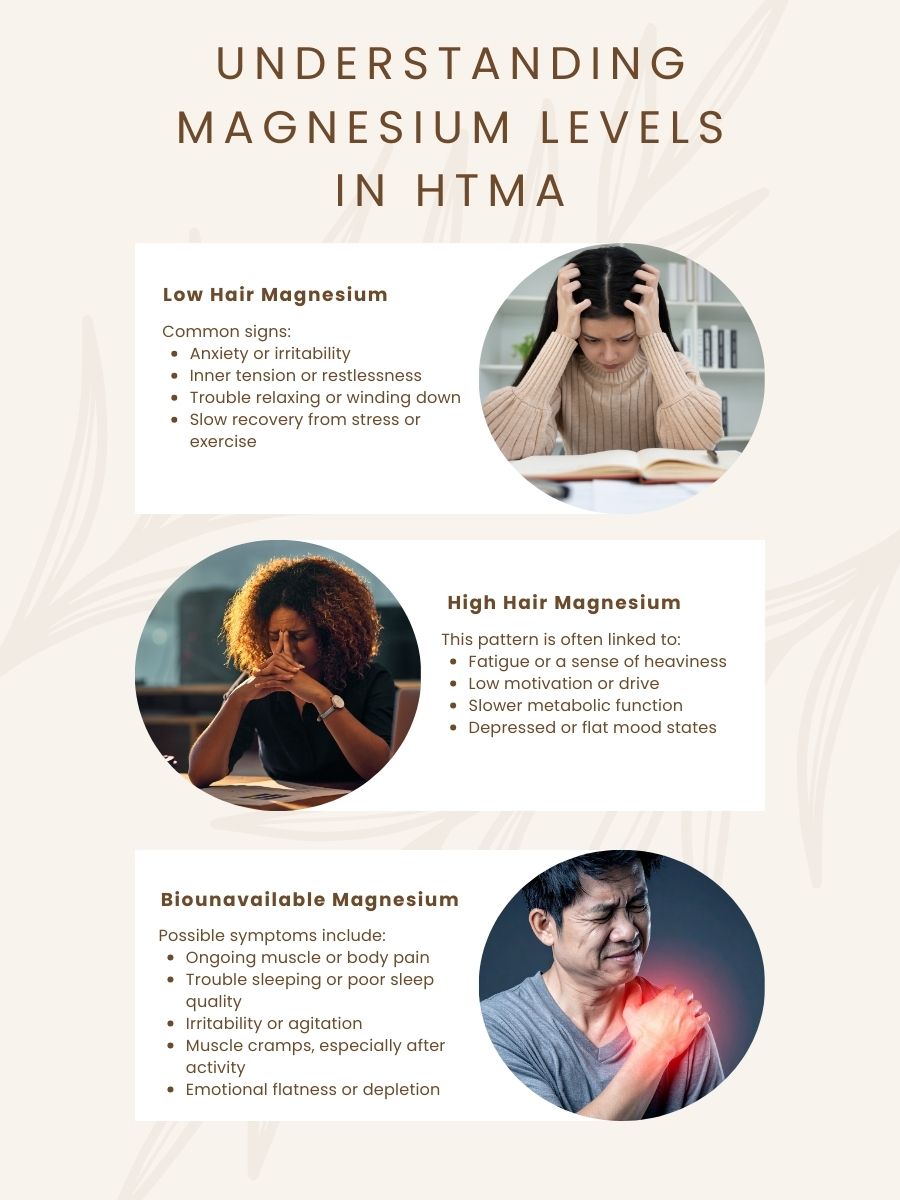
Low Hair Magnesium
Often seen in fast oxidation and high-stress states.
May reflect:
- Increased magnesium loss due to stress
- Higher metabolic demand
- Reduced buffering capacity in the nervous system
Common experiences:
- Anxiety or irritability
- Inner tension or restlessness
- Difficulty winding down
- Poor recovery from stress or exercise
When magnesium drops below ~3 mg%, this often reflects internal pressure and reactivity, not aggression — the system is running without enough cushioning.
High Hair Magnesium
More common in slow oxidation and exhaustion patterns.
In many cases, magnesium is present in the tissues but not biologically available.
This pattern may be associated with:
- Fatigue or heaviness
- Low motivation or drive
- Sluggish metabolism
- Depressive or flat mood states
High magnesium does not automatically mean adequacy.
Biounavailable Magnesium
When hair magnesium rises above ~10 mg%, part of it often exists in an unusable (“amigo”) form.
This form:
- Cannot support enzymes effectively
- Acts as an irritant rather than a stabilizer
- Accumulates in tissues instead of supporting energy
Symptoms may include:
- Chronic muscle or body pain
- Insomnia or poor sleep quality
- Irritability or agitation
- Muscle cramps after activity
- Emotional dullness or depletion
This pattern often reflects adrenal depletion and long-term stress adaptation.
High vs Low vs Biounavailable Magnesium (HTMA Table)
| Magnesium Pattern | Common Symptoms & Experiences | What It Often Indicates in HTMA |
| Low Magnesium | Nervous tension, irritability, muscle tightness, poor sleep, stress sensitivity | Increased magnesium loss due to stress, fast oxidation, higher metabolic demand |
| High Magnesium | Fatigue, low drive, heaviness, slowed metabolism | Slow oxidation, exhaustion stage of stress, magnesium present but poorly utilized |
| Biounavailable Magnesium | Chronic pain, insomnia, irritability, post-exercise cramps, emotional flatness | Magnesium locked in unusable forms, adrenal depletion, impaired enzyme activity |
Important:
Magnesium levels must always be interpreted with ratios, oxidation rate, and trends over time.
Magnesium, Oxidation Rate & Stress
Magnesium patterns closely mirror how the body handles stress.
Fast oxidizers
- Lose magnesium rapidly
- Often feel “wired but tired”
- May need magnesium support even if levels look normal
Slow oxidizers
- Often show elevated hair magnesium
- Magnesium may be present but unavailable
- Experience fatigue, low thyroid signaling, and slow recovery
The Ca/Mg and Na/Mg ratios help clarify whether magnesium is being used, lost, or stored defensively.
Stress, Inner Pressure & Magnesium Depletion
Magnesium is often described as the body’s buffer mineral. It helps the nervous system absorb pressure, regulate impulses, and recover from stress.
When magnesium is adequate and bioavailable, stress is easier to tolerate and recovery is smoother. When magnesium is depleted or unavailable, that buffering capacity is reduced — reactions become sharper, rest becomes harder, and internal pressure builds even when external demands have not increased.
Over time, sustained internal strain can lower tissue magnesium levels. This does not always appear as anxiety. More often, it shows up as reduced nervous system flexibility.
Common signs may include:
- Irritability or poor impulse control under stress
- Restlessness or difficulty settling the body and mind
- Reduced emotional responsiveness or motivation
- Feeling drained rather than calm or alert
HTMA researcher and psychologist Dr. Rick Malter described a related stress pattern he called “The Judge” — a persistent internal state of self-criticism, pressure to perform, and mental over-control. This ongoing inner vigilance keeps the nervous system activated and accelerates cellular magnesium loss.
When this pattern persists, the impact is not only emotional. Reduced magnesium buffering increases physiological strain and can interfere with stress tolerance, learning, and emotional regulation — particularly in children and in adults under sustained demand.
On HTMA, this may appear as:
- Low magnesium relative to calcium
- Rising calcium-to-magnesium (Ca/Mg) ratios
- Slower recovery from stress and reduced resilience
Key insight:
Magnesium depletion is not only dietary. It reflects how stress — especially internal pressure — is carried and processed over time. Supporting magnesium availability helps restore the body’s capacity to regulate, recover, and adapt.
What Magnesium Changes Mean on a Retest
HTMA is about patterns and trends, not single results.
- Rising magnesium may reflect elimination of inferior magnesium compounds
- Falling magnesium may indicate improved utilization rather than loss
- Temporary shifts are common during healing and detox phases
What matters most:
- Direction over time
- Ratio movement
- Symptom changes
A retest provides context that a snapshot cannot.
Factors That Deplete or Block Magnesium
Common contributors include:
- Chronic stress
- Alcohol
- High-sugar or processed diets
- Fluoride and excess phosphorus
- Low protein intake
- Certain medications (stimulants, diuretics, calcium channel blockers)
- Hormonal influences, including estrogen dominance
Key synergists:
- Vitamin D
- Potassium
- Zinc
- Taurine
- Vitamin B6
Magnesium Supplementation in Context
Based on HTMA patterns, magnesium may be used to:
- Support energy production
- Improve stress resilience
- Prevent calcium buildup
- Calm nervous system reactivity
- Support adrenal recovery
Supplementation works best when:
- Balanced with calcium
- Paired with food-based sources
- Guided by HTMA patterns, not symptoms alone
FAQs: Magnesium in HTMA
Can magnesium be high and still deficient?
Yes. High hair magnesium often reflects biounavailable magnesium.
Why doesn’t blood magnesium show this?
Blood levels are tightly regulated and don’t reflect tissue function.
Is magnesium always calming?
Only when it’s bioavailable and properly balanced.
Do I need magnesium even if I supplement?
Often yes — stress, hormones, and metabolism affect retention and use.
Final Takeaway
Magnesium is foundational to energy production, nervous system stability, and stress resilience.
HTMA reveals not just how much magnesium is present, but how your body is adapting under pressure. When interpreted alongside calcium, sodium, and potassium, magnesium becomes one of the clearest indicators of metabolic capacity and long-term resilience.
Understanding your magnesium pattern helps move beyond symptom management — toward restoring true physiological balance.
