Chronic fatigue isn’t just feeling tired.
It’s the kind of exhaustion that doesn’t improve with sleep, rest days, vacations, supplements, or “taking it easy.” It can feel like your body is running on 10% battery… and no one can tell you why.
If you’ve ever thought:
- “Why am I still exhausted after sleeping?”
- “Why do I crash after simple things?”
- “Why do my labs look fine, but I feel awful?”
You’re not alone. And you’re not imagining it.
Article Contents
- What Is Chronic Fatigue
- Why It’s Often Missed
- Symptoms People Don’t Talk About Enough
- The “Low Battery” Analogy That Explains Everything
- Why Many People Are Tired (Start Here First)
- The Real Root Causes (It’s Usually More Than One)
- Mitochondria, ATP, and the Bigger Energy Pathway
- Where HTMA Fits (and Why It Helps)
- What Recovery Looks Like
- Practical Guidelines That Actually Help
- Next Steps: If You Want a Clearer Map
What Chronic Fatigue Really Is
Chronic Fatigue Syndrome (CFS)—also called ME, post-viral fatigue, or CFIDS—is most often defined by one main feature:
Persistent, unrelenting fatigue that isn’t resolved by rest, sleep, or time off.
Many people also experience:
- brain fog (memory and focus problems)
- sleep disturbances
- digestive issues
- body aches or joint pain
- anxiety, low mood, or emotional flatness
These may be secondary effects of the same deeper problem: low adaptive energy.
A note on “energy” (this matters)
When I use the word energy, I’m not talking about motivation or willpower.
Energy, in this context, refers to the body’s ability to supply your cells with ATP (adenosine triphosphate)—your cellular “fuel.” Think of ATP as the refined gasoline that powers your organs, immune response, digestion, detoxification, hormones, and brain.
Dr. Hans Selye called this adaptive energy: the energy your body needs to cope with stress and recover. When adaptive energy is low, even small stressors feel massive.
Why Chronic Fatigue Is Often Missed
One of the most frustrating parts of chronic fatigue is being told:
“Your tests are normal.”
That’s because many standard lab tests show what’s happening in the blood right now, not what has been happening in the tissues over time.
Chronic fatigue is often a long-term pattern, not a single lab abnormality. That’s one reason people keep searching… and searching… and searching.
This is also where Hair Tissue Mineral Analysis (HTMA) can be helpful. It offers a longer-range look at mineral and stress patterns that influence energy production, nervous system function, and detox capacity.
(HTMA is not a disease diagnosis. It’s a functional assessment tool that helps map stress and depletion patterns.)
Symptoms People Don’t Talk About Enough
The hallmark symptom is obvious: exhaustion that doesn’t lift.
But many people also live with:
- “wired but tired” energy (tired body, busy mind)
- crashes after minor activity or socializing
- brain fog that makes you feel “not like yourself”
- sugar cravings or shakiness when meals are delayed
- poor digestion (bloating, constipation, low appetite)
- frequent infections or slow recovery from illness
- anxiety or low mood that feels secondary to exhaustion
What distinguishes chronic fatigue from “ordinary fatigue” is often the timeline:
It persists despite trying—despite effort, supplements, therapies, and lifestyle changes.
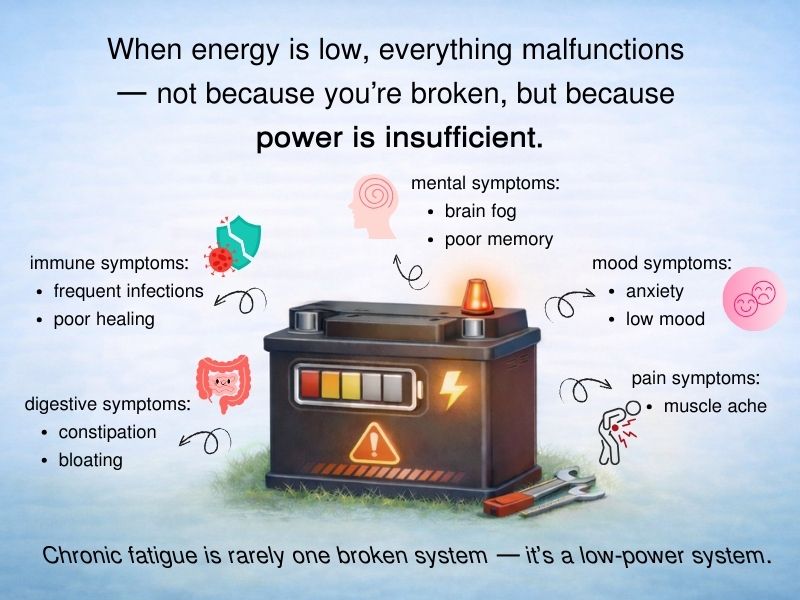
The “Low Battery” Analogy That Explains Everything
Think of newer cars with power steering, power windows, power locks, and electronics everywhere.
When the battery is strong, everything works.
When the battery gets weak, the car doesn’t just develop one problem. It can develop ten—all because the power supply is low.
Chronic fatigue works similarly.
When your body’s energy supply is low, you can get:
- mental symptoms
- digestive symptoms
- immune symptoms
- mood symptoms
- pain symptoms
Not because you’re broken—but because the system doesn’t have enough usable fuel to run smoothly.
Why Many People Are Tired (Start Here First)
Before you assume you have a complex chronic fatigue picture, start with the basics—because sometimes the “obvious” factors are the missing ones.
1) Rest and sleep timing
Many people need 9–10 hours of sleep consistently.
And for many, the timing matters as much as the hours:
- going to bed earlier tends to be more restorative than sleeping late
- frequent night waking reduces recovery
If you’re sleeping “enough” but waking unrefreshed, that’s important data—not a personal failing.
2) Sleep apnea
If you snore, wake with dry mouth, feel unrefreshed, or have daytime sleepiness, sleep apnea can be a hidden cause. It’s worth ruling out with a qualified clinician.
3) Medication-related fatigue
A surprising number of medications can contribute to fatigue, including:
- blood pressure meds
- antihistamines
- antidepressants and anti-anxiety medications
- painkillers and muscle relaxants
- sleep medications
- acid-reducing drugs
If fatigue began after a medication change, that’s worth discussing with your prescribing clinician.
4) Simple nutritional gaps
A diet low in protein and cooked vegetables—or high in sugar/caffeine—can drive fatigue through blood sugar swings and low nutrient intake.
Whole foods, animal protein, and cooked vegetables are a solid start… but for many people with chronic fatigue, it isn’t enough because digestion and absorption are already impaired.
The Real Root Causes (It’s Usually More Than One)
In most chronic fatigue cases, the cause is multiple factors stacking together, such as:
Toxic metals (a major factor)
Toxic metals interfere with thousands of enzyme reactions—many tied directly to energy production.
You don’t need to know which metals you have. Most people carry several due to modern exposure. Nutritional balancing focuses on slow, systematic removal—without chelation—because aggressive chelation often backfires in depleted individuals.
Toxic chemicals
Many people have accumulated chemical exposures from food, water, air, medications, and household products. As energy drops, detox capacity drops—creating a loop.
Nutritional depletion (always present)
Stress increases nutrient needs. Weak digestion lowers absorption. Modern food quality is often reduced. Extreme diets, fasting, raw-heavy eating, vegetarianism in some cases, and refined foods can worsen depletion.
Chronic infections (often opportunistic)
Viruses, fungi, and bacteria can contribute—but often thrive because the body is too depleted to clear them efficiently.
Adrenal and glandular strain
Adrenal and thyroid imbalances can contribute to fatigue, but the deeper issue is often that glands are:
- nutritionally depleted
- slowed by toxins
- strained by nervous system imbalance
Medical and recreational drugs
Many people report fatigue beginning after antibiotics, surgery/anesthesia, or long-term medication use. Drugs can be stored in tissues and contribute to sluggishness until the body rebuilds detox capacity.
Lifestyle and emotional stressors
Chronic worry, relationship stress, financial pressure, anger, fear, guilt, or depression aren’t “just mental.” They create physiological stress and consume adaptive energy.
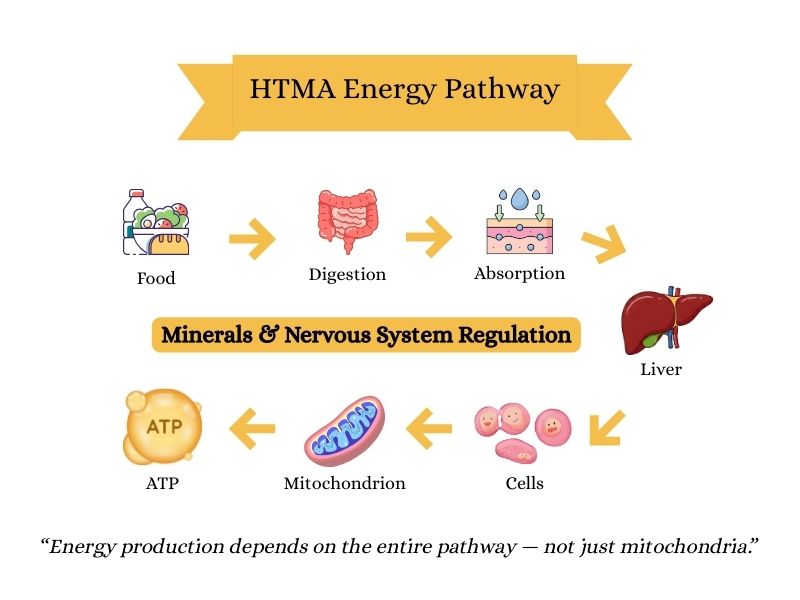
Mitochondria, ATP, and the Bigger Energy Pathway
You’ll hear chronic fatigue explained as “mitochondrial dysfunction.” That’s partly true—mitochondria produce ATP.
But focusing only on mitochondria can miss the bigger picture:
Before mitochondria can make ATP efficiently, your body must move fuel through the entire energy pathway:
eat → digest → absorb → liver processing → deliver nutrients into cells → make ATP → remove waste
If any step is sluggish, energy drops.
This is why people can take “mitochondrial supplements” and still feel exhausted: the upstream steps may still be blocked—especially digestion, liver processing, and cellular mineral balance.
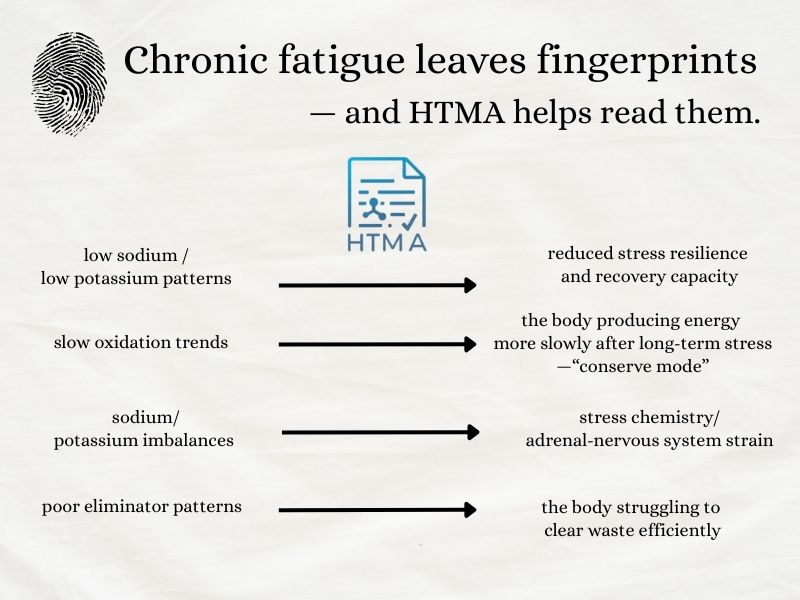
Where HTMA Fits (And Why It Helps)
This is where Hair Tissue Mineral Analysis (HTMA) can be a game-changer—not because it “diagnoses” chronic fatigue, but because it often reveals patterns that explain it.
HTMA helps assess longer-term trends related to:
- mineral reserves
- stress chemistry
- oxidation rate (how fast energy is being produced)
- toxic metal patterns
- detox and elimination capacity
How chronic fatigue often shows up on HTMA
In chronic fatigue cases, we commonly look for patterns such as:
- low sodium / low potassium patterns (reduced stress resilience and recovery capacity)
- slow oxidation trends (the body producing energy more slowly after long-term stress—“conserve mode”)
- sodium/potassium imbalances (stress chemistry/adrenal-nervous system strain)
- low phosphorus patterns (often linked with reduced energy production capacity)
- poor eliminator patterns (the body struggling to clear waste efficiently)
The nervous system piece most people miss
Many people with chronic fatigue also show a pattern called sympathetic dominance—overuse of the fight-or-flight system.
When the body is stuck in fight-or-flight:
- digestion is inhibited
- elimination slows
- immune function weakens
- sleep becomes lighter and less restorative
If sympathetic dominance isn’t addressed, progress can be slow or stalled—even with a “perfect” supplement plan.
What Recovery Looks Like (In Real Life)
Recovery from chronic fatigue is usually not about finding the one magic thing.
It’s about rebuilding capacity.
Nutritional balancing is a lifestyle- and diet-based system designed to:
- replenish minerals and nutrients
- support digestion and absorption
- rebalance oxidation rate (metabolic “engine tuning”)
- gently remove toxic metals and chemicals over time
- restore autonomic nervous system function
- strengthen the body’s adaptive energy
This is why it can work when “quick fix” protocols fail: the goal isn’t stimulation—it’s rebuilding.
A safety note about hormones and stimulants
Hormones like cortisol, DHEA, pregnenolone, adrenal extracts, and other glandular stimulants may provide short-term energy—but they often disrupt feedback loops and delay deeper rebuilding.
Likewise, stimulants (caffeine, sugar, “energy” products) tend to give a temporary boost at the cost of deeper depletion.
Practical Guidelines That Actually Help (When You’re This Depleted)
If you’re dealing with chronic fatigue, these principles are often revelatory:
1) Stop treating exhaustion like a discipline problem
Your body needs rebuilding, not “pushing through.”
2) Stabilise before you detox
If “detox protocols” make you worse, it often means your system needs nourishment and calm first.
3) Eat for steady fuel
Regular meals with adequate protein and cooked foods often help stabilise blood sugar and reduce crashes.
4) Sleep earlier, not just longer
Consistency matters. Earlier sleep tends to restore more deeply.
5) Avoid the stimulant trap
Caffeine and sugar can create “function now, crash later.” If you’re already depleted, that pattern keeps you stuck
6) Choose consistency over intensity
Gentle daily habits often outperform intense protocols for chronic fatigue.
7) Use targeted nutritional support — not stimulation
Many people with chronic fatigue need specific nutrients to rebuild energy systems, nervous system function, and mineral reserves. When chosen carefully (often guided by HTMA patterns), nutritional support helps the body recover rather than forcing energy artificially.
Next Steps: If You Want a Clearer Map
If you’ve been tired for months or years and nothing has helped, the most relieving thing is often not a new supplement—it’s finally understanding why your body feels this way.
Hair Tissue Mineral Analysis (HTMA) can help reveal:
- long-term mineral depletion patterns
- stress chemistry and nervous system trends
- oxidation rate (metabolic “engine speed”)
- toxic metal stress
- elimination/detox capacity
Most importantly, it can help clarify what your body needs right now—and how gently you need to rebuild.
👉 If you want to explore HTMA and nutritional balancing support, this can be a practical next step.
This content is for educational purposes only and is not intended to diagnose, treat, or cure disease.

