
What does high calcium mean on HTMA?
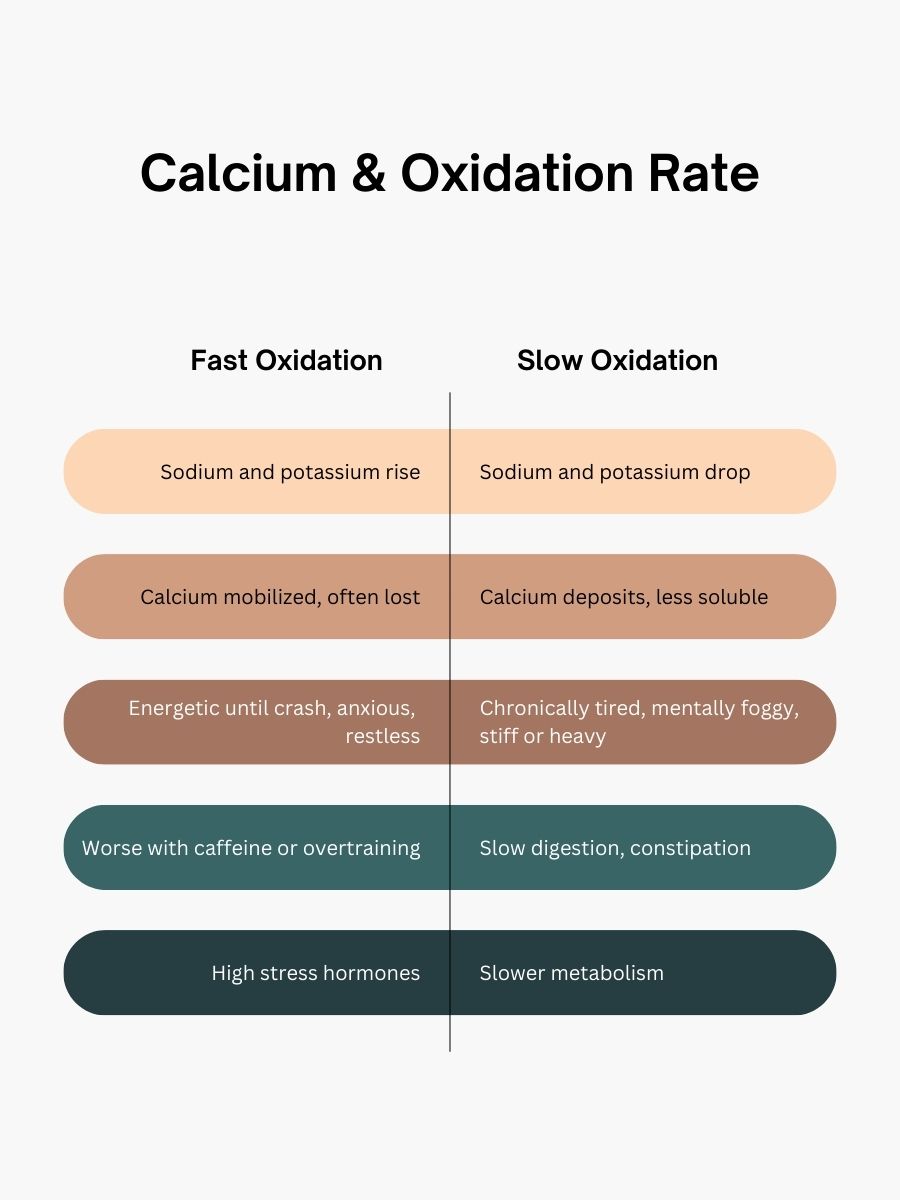
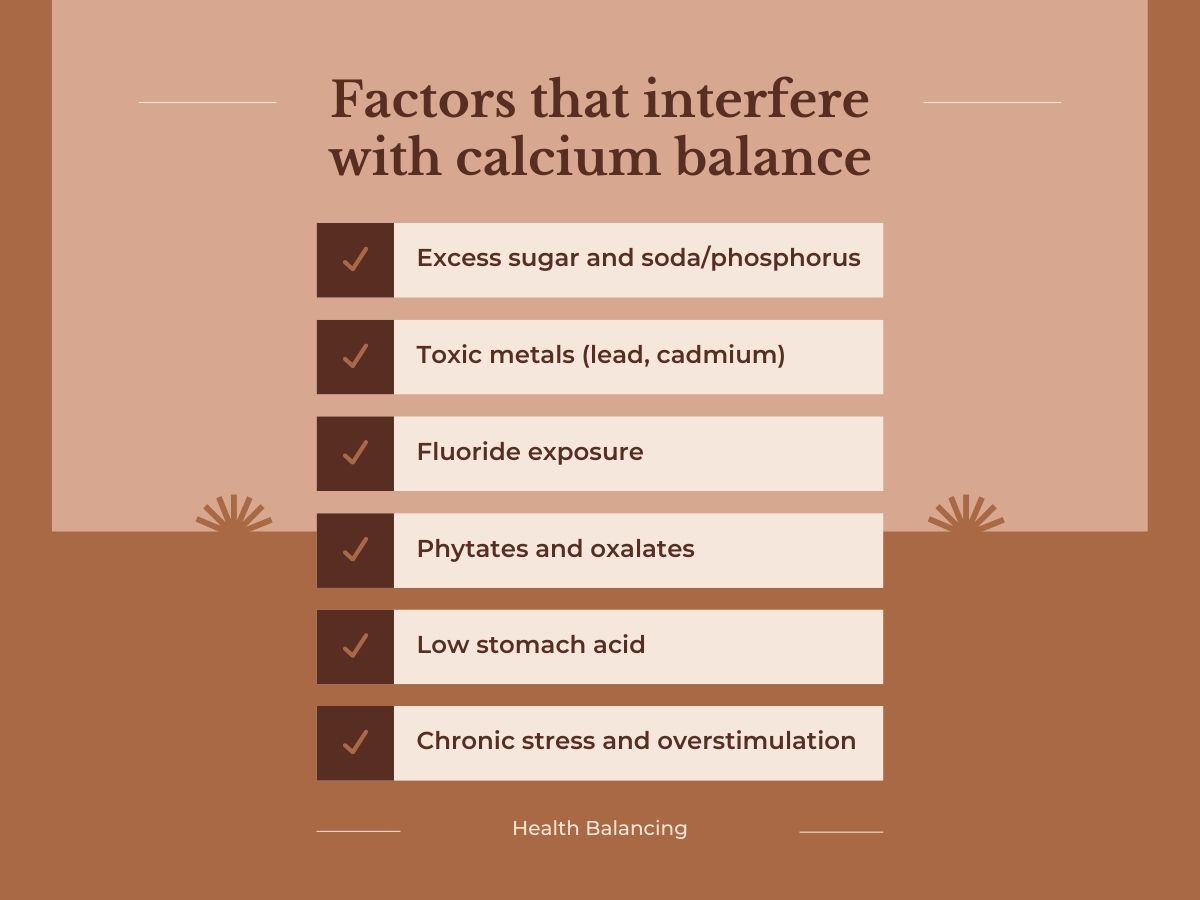
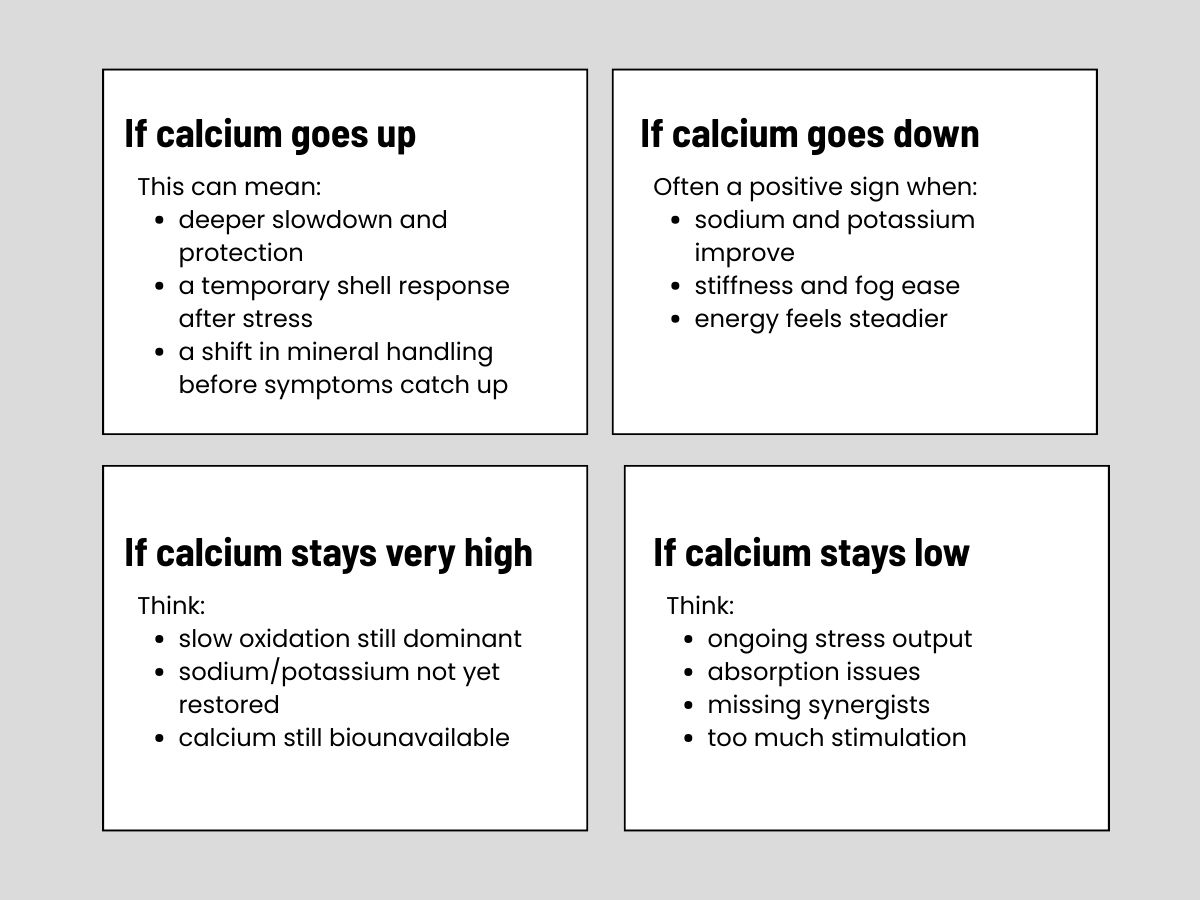
High calcium often reflects slow oxidation and biounavailable calcium, especially when sodium and potassium are low.
What does low calcium mean on HTMA?
Low calcium is commonly seen in fast oxidation and can reflect stress-driven calcium loss.
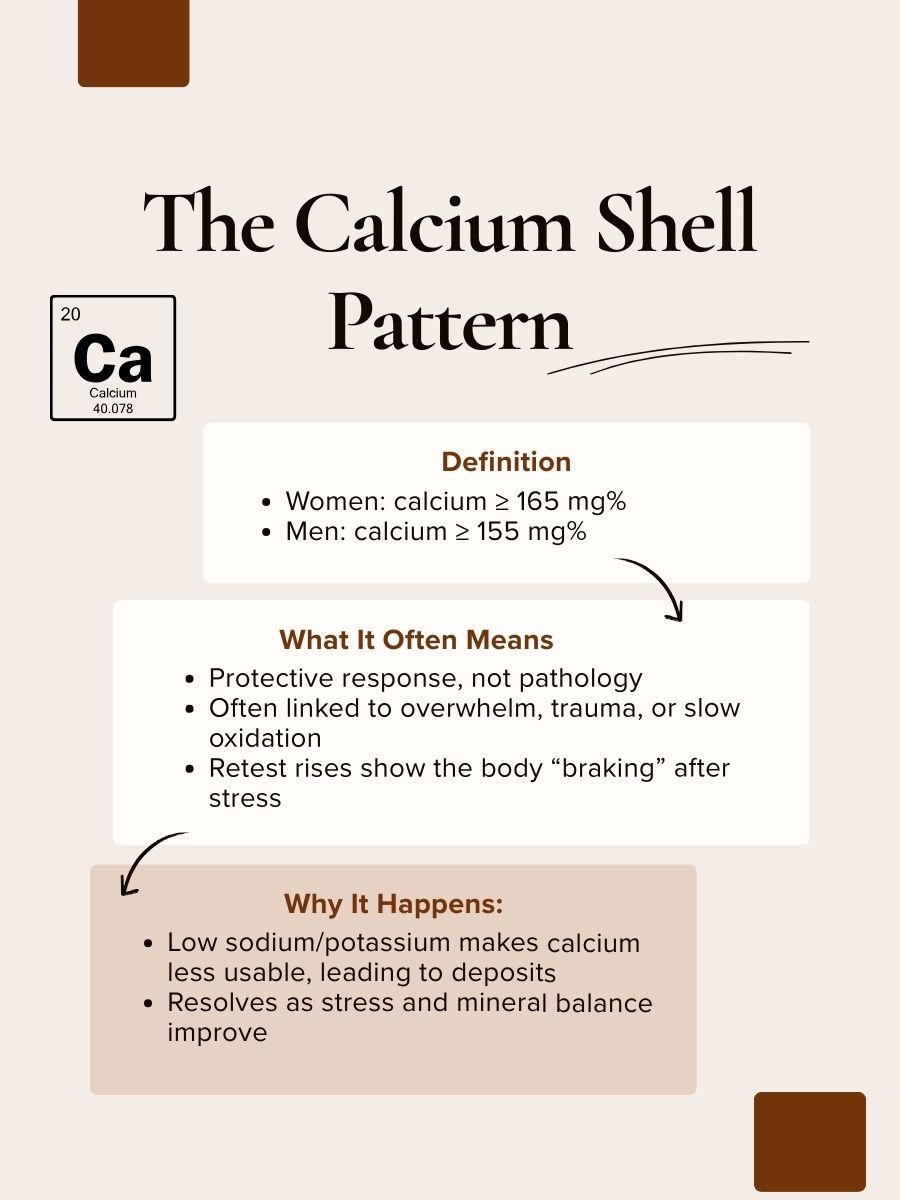
What is a calcium shell?
A calcium shell is a protective HTMA pattern marked by very high calcium, often linked to overwhelm, slow metabolism, and reduced stress tolerance.
Why is my blood calcium normal?
Blood calcium is tightly controlled and doesn’t reflect tissue balance. HTMA looks at longer-term patterns.
Should I supplement calcium?
Sometimes—but only with context. Calcium decisions depend on oxidation rate, ratios, sodium/potassium, and symptoms.
