Why aluminum shows up so often on hair tests — and how stress, digestion, and elimination capacity determine its impact on the brain
Article Contents
- Introduction: Why aluminum deserves attention
- Why aluminum exposure is now unavoidable
- Aluminum and the brain: why cognition is affected first
- Aluminum, attention deficit & child development
- Common symptoms linked to aluminum burden
- Detecting aluminum: blood vs. hair
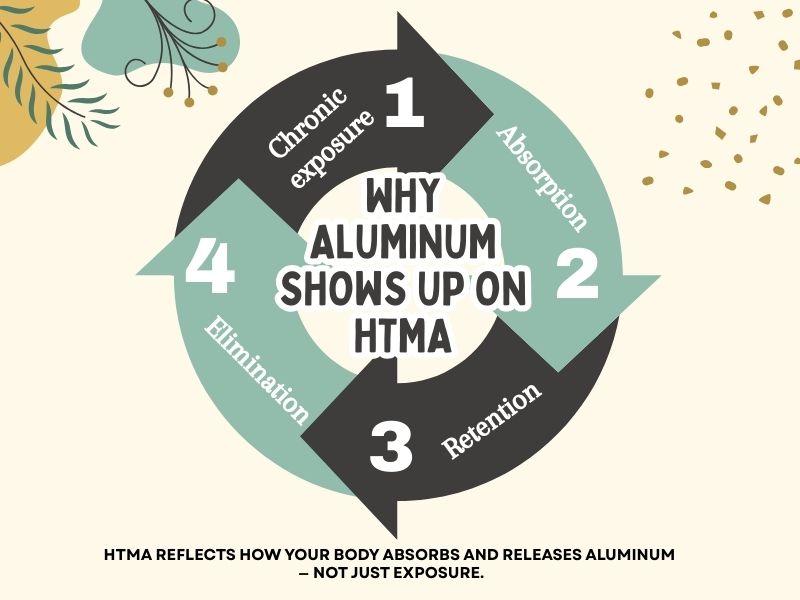
- How aluminum appears on HTMA
- Hidden aluminum toxicity & poor elimination patterns
- Stress, absorption, and why aluminum accumulates
- Supporting aluminum elimination safely
- Key takeaways
Introduction: Why aluminum deserves attention
Aluminum is one of the most consistently elevated toxic metals on Hair Tissue Mineral Analysis (HTMA).
In practice, it appears on the vast majority of hair tests — across ages, diets, and lifestyles.
This does not mean everyone is being “poisoned” in an acute sense.
It means aluminum exposure is chronic, cumulative, and closely tied to stress physiology.
Aluminum is sometimes referred to as the “soft-in-the-head” mineral because it affects the brain and nervous system more than any other system. When aluminum accumulates, people often describe:
- mental fog
- difficulty focusing
- memory lapses
- feeling mentally “slower” or less sharp
HTMA helps us see not just exposure, but whether the body is absorbing, retaining, or eliminating aluminum — which is where symptoms begin to make sense.
Why aluminum exposure is now unavoidable
Aluminum is the most abundant metal in the earth’s crust, and modern processing dramatically increases how much of it enters the body.
Common sources include:
- Drinking water, where aluminum compounds are used in treatment
- Foods prepared with water, including breads, sauces, baby foods, canned and packaged products
- Table salt and processed foods, due to aluminum-based anti-caking agents
- Antiperspirants and deodorants, which use aluminum salts to block sweating
- Vaccines, where aluminum is used as an adjuvant
- Baking powders and baked goods
- Antacids containing aluminum compounds
- Clay-based supplements (bentonite, zeolite, montmorillonite)
- Aluminum cookware and cans, especially with acidic foods
- Cosmetics and skin products
Aluminum also crosses the placenta, meaning many individuals are born with aluminum already present in tissues.
Because exposure is so widespread, the key issue is no longer avoidance alone — it is how well the body handles aluminum once exposed.
Aluminum and the brain: why cognition is affected first
Aluminum has a strong affinity for nervous tissue.
Research and clinical observation show that aluminum can:
- interfere with nerve signal transmission
- inhibit important brain enzymes
- disrupt neurotransmitter uptake
- slow electrical activity in nerve cells
This is why aluminum has been implicated in Alzheimer’s disease and other dementias. However, its cognitive effects are not limited to older adults.
Long before dementia becomes a concern, aluminum may contribute to subtle but impactful changes in mental clarity, memory, and processing speed.
Aluminum, attention deficit & the developing brain
Aluminum can affect mental functioning across the lifespan, including in children.
In practice, aluminum burden is often associated with:
- poor concentration
- attention deficit and distractibility
- learning difficulties
- memory challenges
- slowed cognitive processing
This is especially relevant because exposure often begins early. Many children are born with aluminum, and additional exposure can occur through:
- beverages consumed from aluminum cans
- food cooked in aluminum cookware
- aluminum added to tap water
- aluminum-containing table salt and processed foods
From an HTMA perspective, these effects are often functional rather than permanent. Aluminum does not usually destroy cognitive capacity — it suppresses neurological efficiency while present.
The encouraging point is that aluminum-related attention and cognitive issues are often reversible when aluminum is gradually eliminated and when digestion, mineral balance, and stress physiology are supported.
Common symptoms linked to aluminum burden
Symptoms tend to develop slowly and are often mistaken for stress, aging, or “just how I am.”
Early patterns may include:
- brain fog
- headaches
- flatulence or digestive sluggishness
- heartburn or frequent antacid use
- dry skin and mucous membranes
- frequent minor infections
Longer-term or higher-burden patterns may include:
- memory loss or confusion
- attention and learning difficulties
- neuromuscular weakness
- bone or mineral density issues
- chronic fatigue
- mood and concentration instability
Aluminum rarely acts alone — it often compounds other stressors.
Detecting aluminum: blood vs. hair
Blood aluminum
- May reflect recent exposure
- Does not correlate well with total body burden
- Often appears normal despite tissue accumulation
Hair aluminum (HTMA)
- Correlates more closely with bone and tissue levels
- Reflects aluminum the body is attempting to eliminate
- May require repeated tests to reveal deeper patterns
Because aluminum can be tightly stored in tissues, a single test may not show the full picture — especially when elimination is impaired.
How aluminum appears on HTMA
HTMA interpretation focuses on patterns, not just numbers:
- absolute aluminum level
- trends over time (rising vs. falling)
- relationship with stress and metabolic minerals
- evidence of elimination vs. retention
A rise in aluminum on a retest during nutritional balancing is often a positive sign, indicating mobilization from deeper storage sites.
Hidden aluminum toxicity & poor elimination patterns
Aluminum toxicity can be hidden on HTMA.
Clues that aluminum is being retained even when hair levels look low include:
- a poor eliminator pattern
- elevated iron and manganese, which often travel with aluminum
- stress-related mineral imbalances
In these cases, low aluminum on hair does not mean low aluminum in the body — it often means the body cannot excrete it yet.
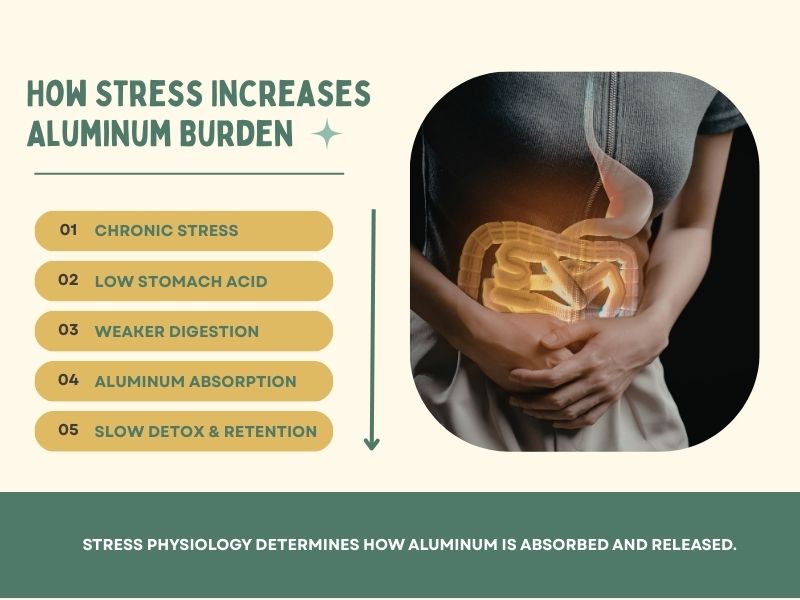
Stress, absorption & why aluminum accumulates
Aluminum accumulation is closely tied to stress physiology.
Chronic stress can:
- reduce stomach acid and digestion
- increase intestinal permeability
- impair liver, kidney, and skin elimination
- suppress sweating
When digestion weakens and elimination slows, aluminum absorption increases and clearance decreases.
This is why aluminum often appears alongside:
- adrenal burnout patterns
- sympathetic dominance
- low sodium and potassium
- slow metabolic rates
Supporting aluminum elimination safely
Aluminum does not require aggressive detox.
In most cases, it responds well to foundational support, including:
- adequate rest and sleep
- improved digestion and mineral absorption
- repletion of antagonists such as calcium, magnesium, zinc, and vitamin C
- gentle sweating support when appropriate
- reducing ongoing exposure where practical
Chelation drugs exist for aluminum but carry risks and are rarely necessary. For most people, aluminum clears as overall metabolic and stress balance improves.

Key takeaways
- Aluminum is extremely common and often overlooked
- It affects the brain and attention regulation early
- Children can be affected, often from early-life exposure
- Cognitive and attention effects are often reversible
- Blood testing frequently misses aluminum burden
- HTMA reveals aluminum in the context of stress and elimination capacity
Aluminum is not just an exposure issue.
It is a stress, absorption, and elimination issue — and HTMA helps make that visible.

