Why blood tests often miss the problem — and how HTMA helps explain chronic mercury stress
Article Contents
- Introduction: Why mercury confusion is so common
- Where mercury exposure comes from today
- Why symptoms persist when tests look “normal”
- Blood vs. hair for mercury: what the research actually shows
- How HTMA interprets mercury differently
- The “low mercury” paradox on HTMA
- Why aggressive detox and chelation often backfire
- Supporting safe mercury elimination over time
- Key takeaways
- References (NCBI / PubMed)
Introduction: Why mercury confusion is so common
Mercury is one of the most toxic elements known to human biology.
It is also one of the most misunderstood.
Many people suspect mercury exposure because of symptoms like:
- brain fog
- anxiety or mood changes
- chronic fatigue
- neurological sensitivity
- digestive or immune issues
Yet when they test mercury, they are often told:
“Your blood mercury is normal.”
This creates a frustrating disconnect between how someone feels and what their labs show.
The problem is not that mercury isn’t involved.
The problem is how mercury is measured — and when.
Where mercury exposure comes from today
Most modern mercury exposure is chronic, low-grade, and cumulative, not acute poisoning.
Common sources include:
- Regular consumption of fish and seafood (especially larger predatory fish)
- Dental amalgam fillings (mercury vapor exposure)
- Environmental and industrial contamination
- Household and occupational products
- Congenital exposure (mercury crossing the placenta before birth)
Because exposure is widespread, the more relevant question is no longer if someone has been exposed, but:
Is their body able to safely process and eliminate what it carries?
Why symptoms persist when tests look “normal”
Mercury behaves very differently from many toxins.
According to toxicology research:
- Mercury leaves the bloodstream relatively quickly
- It preferentially accumulates in brain, kidneys, liver, and endocrine tissues
- Once stored, it can remain for years
- It interferes with enzymes, minerals, and nervous system signaling
This explains a common clinical pattern:
- Symptoms suggest toxicity
- Blood tests look reassuring
- Nothing “shows up” clearly
This does not mean mercury is absent.
It means it is no longer circulating.
Blood vs. hair for mercury: what the research actually shows
This distinction is well documented in peer-reviewed literature indexed in NCBI / PubMed.
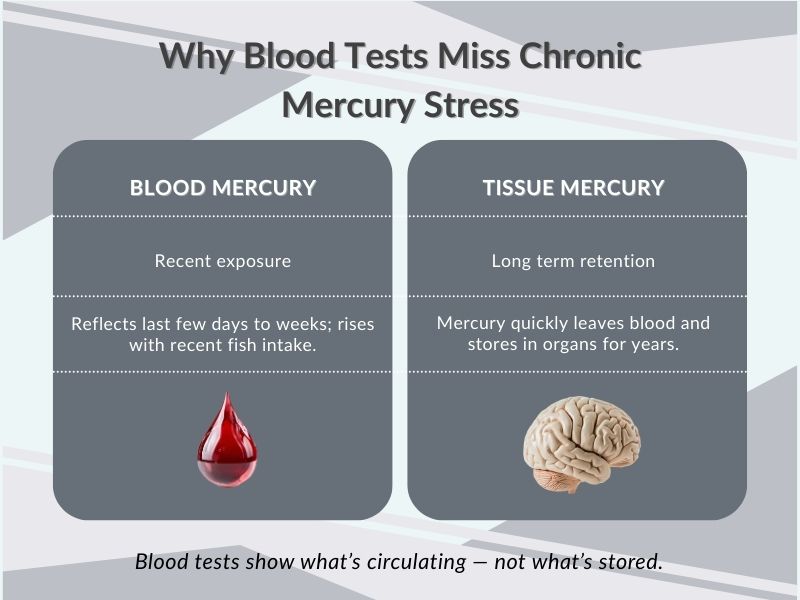
Blood mercury
- Reflects recent exposure (days to weeks)
- Especially useful for identifying current fish intake
- Levels decline relatively quickly when exposure stops
- Poor indicator of long-term retention
Hair mercury
- Mercury binds to keratin as hair grows
- Reflects integrated exposure and elimination over weeks to months
- Once incorporated, mercury does not leave the hair
- Serves as a longer-term biomarker rather than a snapshot
A major NCBI review on mercury biomarkers explains that hair mercury is particularly useful for assessing longer-term methylmercury exposure, while blood primarily reflects recent intake and fluctuates rapidly with diet changes. (Note to nicole, please check which article in section 10 (references) this sentence is referring to. include the relevant link and footnote here e.g. [1] for the 1st reference).
In other words:
- Blood answers: “What happened recently?”
- Hair answers: “What has the body been handling over time?”
This difference is central to understanding chronic mercury stress.
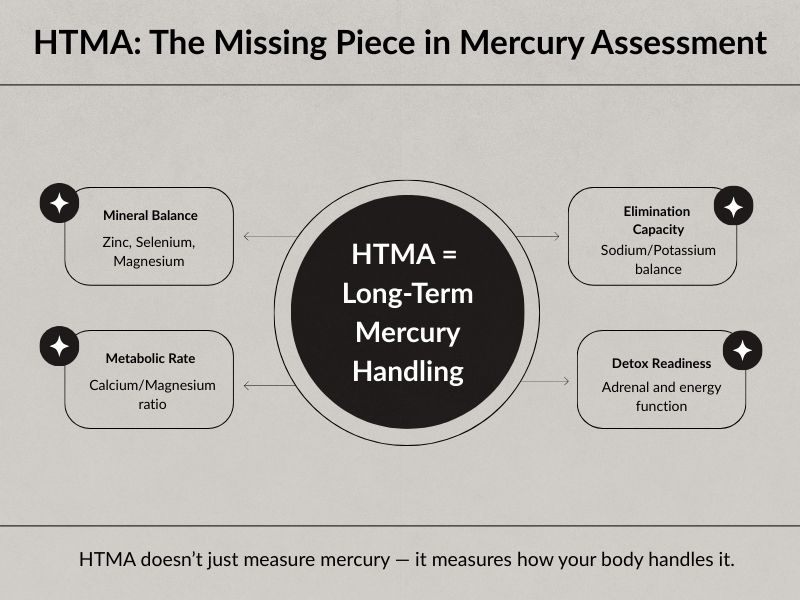
How HTMA interprets mercury differently
Hair Tissue Mineral Analysis (HTMA) does not attempt to measure total body mercury.
Instead, it evaluates:
- Mercury in context
- Alongside mineral status
- Within metabolic and stress patterns
HTMA helps answer questions blood tests cannot, such as:
- Is mercury being excreted at all?
- Is the body retaining mercury instead of eliminating it?
- Are mineral imbalances interfering with detox pathways?
- Is the system too depleted to detox safely?
This pattern-based interpretation aligns with toxicology research showing that mercury toxicity is strongly influenced by mineral interactions, particularly zinc and selenium status.
The “low mercury” paradox on HTMA
One of the most confusing findings for clients is this:
Very low mercury on HTMA does not always mean low mercury in the body.
Research and clinical observation both show that:
- Some individuals retain mercury rather than excrete it
- In these cases, hair mercury can appear deceptively low
- This reflects impaired elimination, not absence
This is why low hair mercury must be interpreted alongside:
- Sodium and potassium (adrenal output and elimination drive)
- Calcium and magnesium (metabolic rate)
- Zinc and selenium (mercury antagonists)
Without this context, mercury results can be misunderstood or falsely reassuring.
Why aggressive detox and chelation often backfire
Chelation is often presented as the solution for mercury toxicity.
However, research and clinical outcomes show several risks:
- Chelators can remove essential minerals along with mercury
- Mercury may be mobilized faster than the body can excrete it
- Redistribution into sensitive tissues (like the brain) can occur
- Symptoms often worsen in depleted or stressed individuals
This is why many people feel worse after “detox protocols” — not better.
Mercury removal is not just about binding the metal.
It is about whether the body has the energy, minerals, and organ function to carry the process through safely.
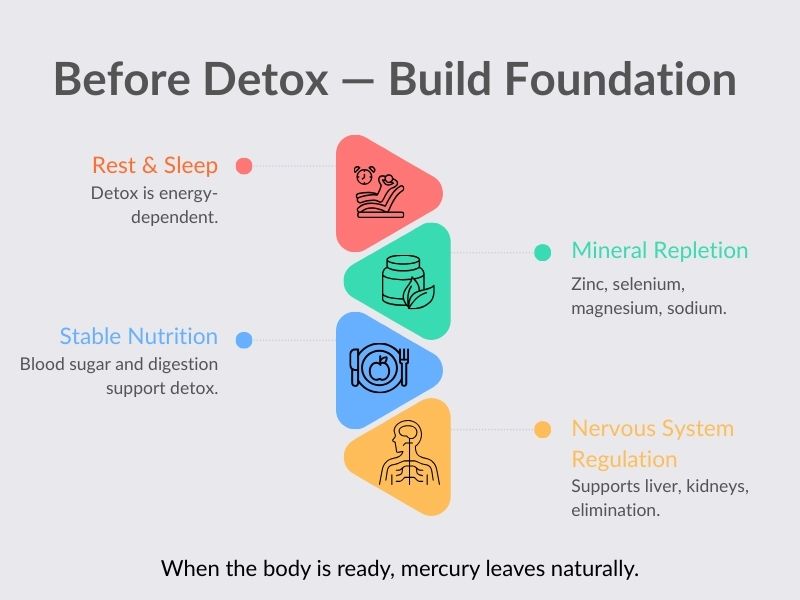
Supporting safe mercury elimination over time
A safer approach focuses on restoring capacity first, not forcing detox.
Key foundations include:
- Adequate rest and sleep (detox is energy-dependent)
- Mineral repletion (especially zinc, selenium, magnesium, sodium)
- Stable blood sugar and digestion
- Gentle skin elimination (when appropriate)
- Nervous system regulation to support liver and kidney function
- Patience and sequencing
When these systems improve, mercury elimination tends to occur gradually and naturally, often without dramatic reactions.
Key takeaways
- Blood mercury and hair mercury measure different things
- Blood reflects recent exposure; hair reflects longer-term handling
- Normal blood mercury does not rule out chronic mercury stress
- HTMA helps assess elimination capacity, not just exposure
- Low hair mercury can signal retention rather than safety
- Timing and readiness matter more than aggressive detox
Mercury is not something to chase.
It is something the body releases when conditions are right.
References (NCBI / PubMed)
Basu N, Horvat M, Evers DC, Zastenskaya I, Weihe P, Tempowski J, et al.
A State-of-the-Science Review of Mercury Biomarkers in Human Populations Worldwide Between 2000 and 2018. Environmental Health Perspectives. 2018;126(10):106001. DOI: 10.1289/EHP3904
https://pubmed.ncbi.nlm.nih.gov/30407086/
Ye BJ, Kim BG, Jeon MJ, Kim SY, Kim HC, Jang TW, et al.
Evaluation of Mercury Exposure Level, Clinical Diagnosis and Treatment for Mercury Intoxication.
Annals of Occupational and Environmental Medicine. 2016;28:5. DOI: 10.1186/s40557-015-0086-8
https://pmc.ncbi.nlm.nih.gov/articles/PMC4724159/
World Health Organization (WHO).
Assessment of Prenatal Exposure to Mercury: Standard Operating Procedures.
Geneva: World Health Organization; 2018. ISBN: 9789240002845
https://www.who.int/publications/i/item/9789240002845